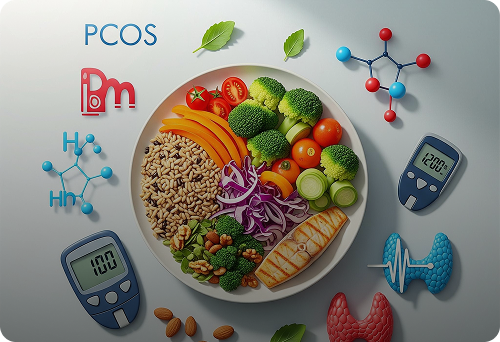
Chronic endocrine disorders such as Polycystic Ovary Syndrome (PCOS), diabetes, and thyroid dysfunction are increasingly prevalent worldwide, significantly impacting quality of life and long-term health outcomes. Nutrition plays a pivotal role in managing these conditions by influencing hormonal balance, metabolic function, and systemic inflammation. For healthcare providers and patients alike, understanding evidence-based nutritional strategies is essential to optimize disease control and improve patient well-being.
Nutrition and Polycystic Ovary Syndrome (PCOS)
PCOS is a multifaceted hormonal disorder affecting reproductive-aged women, characterized by insulin resistance, hyperandrogenism, and ovulatory dysfunction. Nutrition interventions targeting insulin sensitivity and inflammation can profoundly affect symptom severity and fertility outcomes.
- Insulin Resistance and Diet: A central feature of PCOS is insulin resistance, which exacerbates hyperandrogenism. Diets low in refined carbohydrates and high in fiber help stabilize blood glucose levels and reduce insulin spikes. Emphasizing complex carbohydrates, such as whole grains, legumes, and vegetables, supports improved insulin sensitivity.
- Anti-Inflammatory Foods: Chronic low-grade inflammation is commonly observed in PCOS. Incorporating foods rich in omega-3 fatty acids (e.g., fatty fish, flaxseeds), antioxidants (berries, leafy greens), and polyphenols (green tea, turmeric) may reduce inflammatory markers and improve hormonal profiles.
- Weight Management: Even modest weight loss of 5-10% can restore ovulation and improve metabolic parameters. Nutritional counseling focused on caloric balance and sustainable eating patterns is critical for effective weight management in PCOS patients.
Nutrition’s Impact on Diabetes Management
Diabetes mellitus, particularly type 2 diabetes, is a metabolic disorder characterized by chronic hyperglycemia due to impaired insulin secretion and action. Nutrition is a cornerstone of diabetes management, directly influencing glycemic control and risk of complications.
- Carbohydrate Quality and Quantity: Monitoring carbohydrate intake remains essential. Prioritizing low glycemic index (GI) foods—such as legumes, nuts, and non-starchy vegetables—can mitigate postprandial glucose surges. Carbohydrate counting, paired with portion control, empowers patients to maintain blood sugar within target ranges.
- Macronutrient Distribution: Balanced intake of carbohydrates, proteins, and healthy fats supports metabolic health. Protein contributes to satiety and glycemic stability, while monounsaturated and polyunsaturated fats (olive oil, avocados) improve lipid profiles and insulin sensitivity.
- Dietary Patterns: Research supports the efficacy of Mediterranean, DASH (Dietary Approaches to Stop Hypertension), and plant-based diets in diabetes care. These diets emphasize whole foods, healthy fats, and minimal processed ingredients, contributing to cardiovascular risk reduction.
- Micronutrients and Supplements: Certain micronutrients, such as magnesium, chromium, and vitamin D, have shown potential in improving insulin action and glucose metabolism. However, supplementation should be individualized and based on clinical evaluation.
Nutritional Considerations in Thyroid Disorders
Thyroid disorders, including hypothyroidism and hyperthyroidism, impact metabolic rate, energy levels, and systemic function. Proper nutrition supports thyroid health and complements pharmacologic treatment.
- Iodine Intake: Iodine is essential for thyroid hormone synthesis. Adequate iodine consumption through iodized salt, seafood, and dairy supports normal thyroid function. However, excessive iodine intake may exacerbate thyroid dysfunction and should be monitored.
- Selenium and Zinc: These trace minerals are critical cofactors in thyroid hormone metabolism and antioxidant defense. Brazil nuts, seafood, and pumpkin seeds are rich sources and can help maintain thyroid health.
- Goitrogens: Certain foods such as cruciferous vegetables (broccoli, cabbage) contain goitrogens that may interfere with thyroid hormone production when consumed excessively, particularly in iodine-deficient individuals. Cooking these vegetables typically reduces goitrogenic effects.
- Fiber and Medication Absorption: Hypothyroid patients often require levothyroxine replacement. High-fiber diets may impair medication absorption if consumed concurrently, so timing of meals and supplements should be optimized.
Integrating Nutrition into Chronic Endocrine Care
Effective nutritional management in PCOS, diabetes, and thyroid disorders demands personalized approaches grounded in comprehensive assessment. Interprofessional collaboration between physicians, dietitians, and patients fosters tailored interventions that consider comorbidities, cultural preferences, and lifestyle factors.
Digital health platforms like FriskaAi facilitate this process by leveraging AI-driven nutritional analytics to provide customized meal plans, track adherence, and monitor biometrics. These tools empower patients with actionable insights and support clinicians in delivering precision nutrition as a standard of care.
Supporting Patient Engagement Through Education
Educating patients about the role of nutrition in managing endocrine disorders is critical for sustained behavior change. Clear communication about the benefits of dietary modifications, potential pitfalls, and achievable goals enhances motivation and compliance.
Structured programs combining nutritional counseling with physical activity and psychosocial support have demonstrated superior outcomes in endocrine disease management. Emphasizing small, incremental changes rather than drastic diet overhauls helps foster long-term adherence.
Nutrition remains a foundational component in the management of PCOS, diabetes, and thyroid disorders. By applying evidence-based dietary strategies, healthcare providers can significantly improve patient outcomes, reduce complications, and enhance quality of life.